Pain that is brought on by the thoracic, pelvic, or abdominal viscera's (organs) nociceptors firing. Visceral structures are relatively unresponsive to other stimuli that typically generate pain like cutting or burning but are very sensitive to distension (stretch), ischemia, and inflammation.
Visceral pain is diffuse, difficult to pinpoint, and frequently linked to a far-off structure—usually one that is superficial. It may also be accompanied by symptoms like vomiting, nausea, abnormalities in vital signs, and emotional outbursts. It is possible to describe the pain as dull, squeezing, deep, and terrible.
Only a portion of individuals have specific anatomical lesions or metabolic abnormalities that can account for this sort of discomfort. Gastrointestinal neuromuscular diseases (GINMD) include several conditions.
Others may feel visceral aches, frequently of a very severe character, with no signs of a structural, biochemical, or histopathologic cause.
The pathogenesis and therapy of these illnesses, which are categorized under functional gastrointestinal disorders (FGID), might differ significantly from GINMD. Irritable bowel syndrome and functional dyspepsia are the two main single entities among gut functional diseases.
Visceral hypersensitivity is a phrase used to describe the hypersensitive visceral pain perception that people with functional gastrointestinal problems frequently experience.
What is Visceral Pain?
Visceral pain can be poorly restricted and marked by allergic reactions to a stimulus that includes organ distension. There is a substantial comorbidity between persistent abdominal discomfort and stress-related psychiatric disorders such anxiety and depression.
It is yet unclear how these overlapping comorbidities and visceral pain are related.
According to available data, prolonged stress enhances pain perception and sensitizes pain pathways, creating a feedback loop that encourages chronic visceral pain disorders like irritable bowel syndrome (IBS).
Early childhood stress (ELS) is a risk factor for developing irritable bowel syndrome (IBS), however the processes underlying ELS's enduring impacts on visceral perception in adults are still poorly understood. The causes of stress-induced pain have been studied in mouse models using stress in adult animals produced by restraint and water avoidance.
Symptoms of visceral pain:
Visceral pain can be recognized by its general characteristics, such as deep, aching, squeezing, or colicky sensations that are poorly localized, as well as by their location (such as the belly).
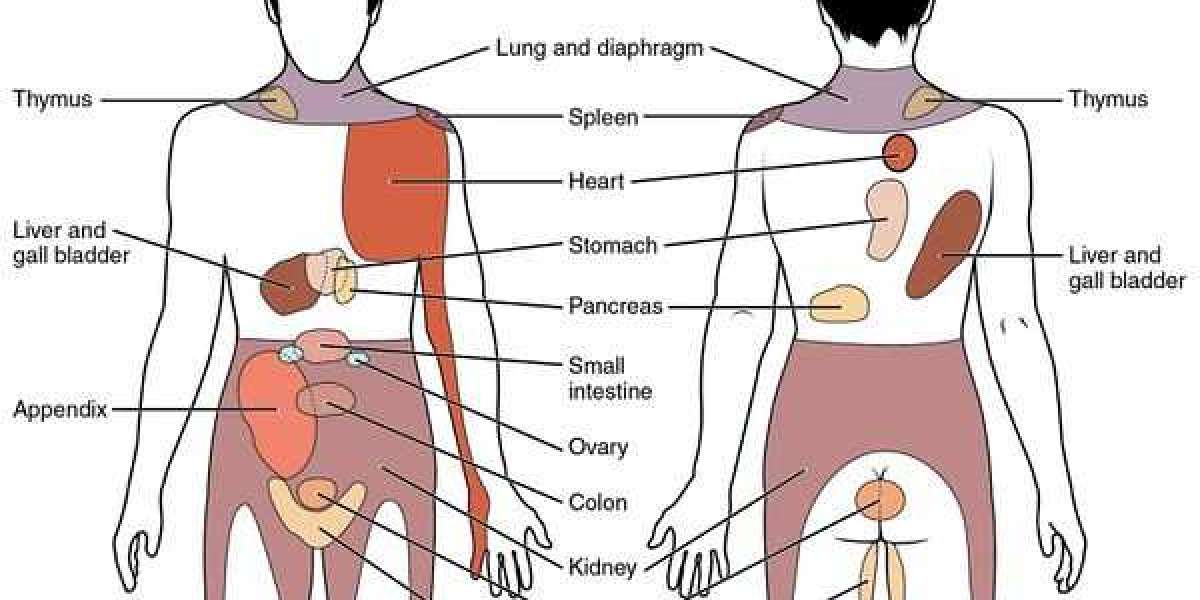
It is frequently referred to as cutaneous sites and is scattered all over the body.
How is visceral pain diagnosed?
Visceral discomfort is frequently experienced at locations far from the actual position of the organ. Many clinicians use this transferred pain, a crucial component of visceral pain, to help diagnose specific disorders.
All viscera cannot produce visceral pain, and there is frequently no connection between internal injury and visceral discomfort.
Even the most harmful stimuli cannot elicit any sensations from some viscera, such as the liver or the kidneys, which are completely indifferent to all forms of stimulation.
Treatment of visceral pain:
We employ a variety of injection therapies since they might be effective as pain specialists.
Patients with untreatable pancreatic cancer or untreatable discomfort from organs including the liver, pancreas, or gallbladder may benefit from a celiac plexus nerve block.
A superior hypogastric plexus block can be very helpful for patients who have chronic, possibly benign, or cancer pain in those areas because the superior hypogastric plexus, another plexus, receives input from organs like the prostate, bladder and uterus.
For example, the vagina in women, or the testes in men.
There is more proof now that spinal cord stimulation can be beneficial. Dorsal column stimulation, for example, can help patients with chronic pelvic pain using a variety of techniques.
It can also help with conditions like pudendal neuralgia, which can cause pain in the perineum, which is the area between a woman's anus and vagina.
For referral purposes, I believe it is crucial that frontline practitioners are aware of such neuromodulator devices.
Read more about other pain - Somatic Pain , Muscle pain